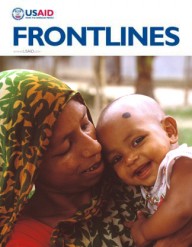
 Enanit Metiku holds her son, Tazen, flanked by Belaynesh Fentie, left, and Tegegnech Tsehay, health extension workers at the Chachi health post, where Tazen was treated.
Vasken Sissian, Tufts University
Enanit Metiku holds her son, Tazen, flanked by Belaynesh Fentie, left, and Tegegnech Tsehay, health extension workers at the Chachi health post, where Tazen was treated.
Vasken Sissian, Tufts University
 Enanit Metiku holds her son, Tazen, flanked by Belaynesh Fentie, left, and Tegegnech Tsehay, health extension workers at the Chachi health post, where Tazen was treated.
Vasken Sissian, Tufts University
Enanit Metiku holds her son, Tazen, flanked by Belaynesh Fentie, left, and Tegegnech Tsehay, health extension workers at the Chachi health post, where Tazen was treated.
Vasken Sissian, Tufts University
In September 2013, Ethiopia announced it had achieved Millennium Development Goal (MDG) 4—reducing child mortality by two-thirds by 2015—a full year ahead of schedule. In 1990, Ethiopia’s under-5 mortality rate was one of the highest in the world at 204 for every 1,000 live births; by 2012, this rate had been slashed to 68 for every 1,000 live births.
“Ethiopia pioneered a strong community health system that has propelled the country to reach this milestone,” says USAID/Ethiopia’s Health Office Chief Elise Jensen. “While this triumph has yielded great benefits for the country as a whole, the individual impact of a child’s life saved cannot be underestimated.”
Last year, Bora Shewki, an 8-month-old Ethiopian boy, was suffering from a poor appetite, cough and fever—symptoms of pneumonia that his mother, Kari Turle, recognized all too well. Kari, a 24-year-old pastoralist, had witnessed more than her fair share of pneumonia, malaria and diarrhea, the most common childhood illnesses in the district of Hamer woreda.
Located in the South Omo Valley, 850 kilometers south of Ethiopia’s capital, Addis Ababa, in the Southern Nations, Nationalities and People’s Region (SNNPR), Hamer woreda, has three health centers and 27 health posts to serve a population of 70,000. Health posts are the closest facilities that provide free preventive and primary curative services to the community; however, they only began treating pneumonia in 2011.
“Before the health post began treating our children and giving us drugs, I took my sick children to the health center, which is very far from where I live,” Kari said. “Then, one morning, the health extension worker in my kebele [subset of woreda/district] came to my house to tell me that she provided treatment to sick children.”
As soon as she noticed Bora’s pneumonia symptoms, Kari brought him straight to the Aera Keysa health post. “In the past, I went to the health post only for vaccination. I am very happy that I don’t have to take my children long distances anymore and the treatment is free of charge,” she said.
Kari’s baby boy recovered from his bout of pneumonia, just as her elder child, 3-year-old Liku Shewki, recovered from malaria as soon as she was treated at the health post six months earlier.
A couple years ago, health posts in Hamer began providing Integrated Community Case Management (iCCM) services, a strategy to expand access to lifesaving treatments for children suffering from common illnesses like Bora’s struggle with pneumonia. After health extension workers (HEWs) attended an iCCM training, they informed families in their communities about these new services by going house to house and hosting vaccination days.
Prior to iCCM, most sick children were treated at distant health centers, with high transport costs and long waiting times. Many families were unable to afford transport, and therefore did not seek the appropriate care for their children, which resulted in more severe illnesses and a greater number of childhood deaths.
Tarikua Lulayehu is the health extension worker in Aera Keysa kebele that likely saved Bora’s life. She proudly reports that Aera Keysa is one of the model kebeles in Hamer woreda because it has successfully applied all 16 health extension program elements, such as routine immunization, hygiene, latrine making and family planning. The availability of these services has reduced the need for referrals, which would often result in kids not receiving treatment due to the time and money required to travel further.
Tarikua says, “Before I attended the iCCM training, I did not have the skills to treat sick children, especially those who suffered from pneumonia. All I did was send them to the health center with a referral slip. Now that I have the skills, I assess and treat sick children and provide medication as necessary. I write referrals only for severe cases. The community has more confidence in the curative service at the health post and I have gained increased job satisfaction as I am now able to help increased numbers of little children in the kebele.”
Community Health Focus
Health extension workers like Tarikua form the backbone of Ethiopia’s health care system. About a decade ago, the Government of Ethiopia rolled out the Health Extension Program (HEP), which trains young women to provide basic health services and deploys them in pairs to rural villages around the country where they can alert communities to unhealthy practices and empower families to take charge of their own health. Unlike traditional health volunteers, HEWs are paid a nominal salary of 700 birr per month ($36) and are considered government employees.
“Our government has a policy of reaching the hard-to-reach parts of the country and focusing on prevention of disease, health promotion and transferring responsibility to individual families,” said Dr. Kesetebirhan Admasu, Ethiopia’s minister of health.
“I believe it is the work of these amazing community health workers who have really put the country to achieve these results,” he said, referring to MDG 4.
Each HEW is assigned on average 500 households, and is also responsible for coordinating with the Health Development Armies (HDAs), a group of unpaid volunteer women who are influential community members, and assist with mobilizing and spreading key health messages in the community.
Since Tarikua and her colleagues began providing iCCM services two years ago, they have assessed and treated 316 children in Aera Keysa kebele and referred 37 cases to a health center.
Tegegn Hussien, deputy head of the Hamer Woreda Health Office, says “iCCM is a national initiative aimed at reducing under-5 mortality and morbidity, and Hamer woreda has not been left behind. Through the initiative, more than 11,040 children under 5 in our woreda have access to curative services to the most common childhood illnesses.”
Since iCCM services began two years ago in Hamer woreda, over 5,760 children have been assessed and treated at health posts. Not only do these services treat children earlier and closer to home, but they also help reduce the case burden of the under-5 clinic in the three health centers.
Childhood Nutrition
In contrast to the arid, pastoralist areas of Hamer woreda, many areas of the Amhara region are filled with agriculturally productive, green highlands where the food supply is secure. Despite some progress in undernutrition and a favorable climate, malnutrition persists as one of the most devastating ailments contributing to child mortality in Ethiopia, indirectly responsible for 45 percent of child deaths each year.
Three-year-old Tazebew “Tazen” Aderajew Adgo used to spend long days without any food in the field where his mom, Enanit Metiku, worked in Chachi kebele, Amhara. Tazen started losing weight, cried from hunger, and began to look sickly. Fearing her husband, who forbade Enanit from feeding Tazen more often, she silently endured the pain of her hungry child, until she could no longer.
“My baby cried. He was fussy all the time, never played or smiled. I knew he was hungry, but my husband told me to ignore Tazen’s condition and continue working. I could not bear to see my baby die in front of me, so I filed for a divorce,” she said.
During a routine community health screening, health extension workers Tegegnech Tsehay and Belaynesh Fentie identified Tazen and four other children as being malnourished.
The nearest health facility with the proper treatment was 180 kilometers away in Gondar. However, Tegegnech and Belaynesh appealed to a USAID-funded effort for immediate training to treat the children. In three days, they learned how to assess and screen cases of severe acute malnutrition and how to counsel and manage cases at the health facility level.
Empowered with the necessary skills and renewed confidence, the women rushed back to the kebele to help the five malnourished children, including Tazen. After checking Tazen’s vital signs and conducting a nutritional assessment, they discovered that he was severely malnourished. They treated Tazen with a peanut-based, ready-to-use therapeutic food called Plumpy’Nut, antibiotics, de-worming medicine and iron-folic acid for anemia. After a month, Tazen’s weight, attitude, mood, appetite and sleep patterns all improved.
Enanit recruited help to compose a thank-you letter to the health workers: “Now he smiles, he sleeps well and he plays with his sister,” the letter read. “I am so happy you saved my baby. This is giving life. I now tell every mother in my situation that they can get help at the health post …. You are his family now.”
Since that training workshop, more than 200 children in the district under age 5 have received assistance for childhood nutrition, more than 410,000 in the Amhara region, and more than 1.6 million throughout the country.
Says USAID/Ethiopia Mission Director Dennis Weller: “USAID and our partners in Ethiopia were very excited to announce that Ethiopia has achieved the Millennium Development Goal Four, by reducing child mortality under age 5 by 67 percent since 1990. This success is attributable to the determined leadership and commitment of the Ethiopian Government, and the partnership and support from all stakeholders …. There is still more work to do to make preventable maternal and newborn deaths an issue of the past, but we are hopeful, and know that given our close collaboration with the Ministry of Health, other partners and donors, we will achieve our goals.”
Related Links
The Kangaroo Model
USAID is currently evaluating kangaroo mothercare, or KMC, to help babies born prematurely survive.
Like the mammal it is named for, KMC provides essential thermal care for babies through continuous skin-to-skin contact with a mother, father or other caretaker, and is used for two to three weeks until a baby reaches a normal weight. It is a proven intervention and recommended practice to reduce newborn mortality for preterm and low birth weight babies.
In most countries, the use of incubators is standard for thermal care of preterm and low birth weight babies. However, incubator care is not widely available in developing countries, and even in the limited areas where it is available, maintenance and power outages present challenges. Incubators also largely exclude the participation of the mother, which can lead to decreased breastfeeding and affect maternal-newborn bonding.
Babies who are born premature are around 20 times more likely to die compared to babies who have higher birth weights; and around one-third of low birth weight babies die within the first 12 hours of delivery. Since most deliveries take place at home in Ethiopia, community kangaroo mothercare teaches mothers and other caretakers how to practice prolonged skin-to-skin contact and provide exclusive breastfeeding while they are in their home.
Although in-home practice of kangaroo mothercare is still in the testing phase in Ethiopia, at least one new mom is wise to the wisdom of kangaroos—and has a healthy baby to show for it.
Shortly after delivering her third baby, Alemitu Kelkaye began experiencing difficulties feeding the newborn. Her son was not sucking properly, and she could not produce enough milk.
When she visited health worker Yemiserach Sileshi a few meters from her home at the Mosobo health post in Yilmana-Densa district, Amhara region, Alemitu shared her concerns about the baby’s feeding. The baby was slightly underweight at 2.3 kilograms. So Yemiserach suggested the kangaroo method she had been trained by USAID to deploy in such situations.
She put the newborn in between his mother’s breasts and wrapped them tight with netela gabi, a locally available traditional thick cotton scarf, in the perfect KMC position. The baby was then warm and comfortable—and he began to nurse.
“When I felt my baby relax, I felt happy and relaxed too,” Alemitu said. After two weeks, she says, “he has grown now and he wants to come out.”
Between 2011 and March of this year, 5,022 newborns were kept in the kangaroo positions by their mothers at 89 selected health posts in the Amhara, Oromia, SNNP and Tigray regions. Community KMC is still in the evaluation phase and is being documented by the USAID-funded Maternal and Child Health Integrated Program (MCHIP).
Hannah Gibson, MCHIP Ethiopia project director, says, “Evidence shows us that KMC works. Furthermore, it does not require any special equipment or materials to implement. It is perfectly suited to Ethiopia and we hope that the results of the evaluation will show that it can be easily integrated into the package of counseling services that HEWs provide to pregnant women and newly delivered mothers.”
For her part, Alemitu says she will speak out about the importance of KMC so that other mothers can increase the chances of survival for their newborns.














Comment
Make a general inquiry or suggest an improvement.