Malaria transmission in Ethiopia is unique. Unlike other sub-Saharan African countries, malaria is caused by two malaria parasite species in Ethiopia: Plasmodium falciparum and P. vivax, which account for 60 percent and 40 percent of cases, respectively. Ethiopia’s treatment guidelines recommend artemether-lumefantrine as the first line treatment for P. falciparum and chloroquine for P. vivax malaria. To ensure that patients are appropriately treated with the correct drug, it is important that patients receive quality parasitological diagnosis.
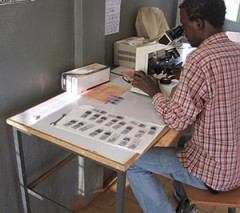
In Ethiopia, parasitological diagnosis of malaria is done using multi-species rapid diagnostic tests (RDTs) at the health post level and microscopy at health centers and hospitals. Although tremendous progress has been made by the Federal Ministry of Health to roll out multi-species RDTs, there remain critical gaps and challenges in malaria microscopy. These include: poor malaria laboratory diagnosis capacity, lack of supplies, and lack of a quality assurance and monitoring system, as evidenced by a baseline assessment conducted in 70 health facilities in five zones of the populous Oromia Region.
PMI/Ethiopia, in close collaboration with the Federal Ministry of Health, the Ethiopian Health Nutrition Research Institute, and the Oromia Regional Health Bureau, has been implementing malaria laboratory diagnosis and monitoring activities for the last three years. This has included developing guidelines and training materials for malaria laboratory diagnosis, training clinical and laboratory health professionals in malaria laboratory diagnosis, and supporting quality assurance/quality control systems.
To date, almost 750 health professionals have been trained in malaria laboratory diagnosis and quality assurance, and an external quality assessment program is currently implemented in 57 facilities. This program provides standard microscopes and related quality laboratory supplies as well as supportive supervision and mentorship. To assess improvement in these 57 PMI-supported health facilities, microscope slides with blood smears from patients with suspected malaria were randomly selected and collected from facilities to be blindly rechecked by senior malaria microscopists. Second and third slide external blind readers were used to ensure that discordant results were further read and final results produced. The first round external quality assessment found a remarkable improvement in the quality of microscopic malaria diagnosis: there was 87 percent agreement between slide readings in the assessment, compared with only 64 percent agreement during the baseline assessment, which was conducted before the intervention.
The 87 percent agreement of rechecked slides is an objective assessment of the laboratories’ concerted efforts to make quality improvements based upon the trainings and guidance provided. Feedback from the external quality assessment was communicated to participating facilities; results were discussed, and follow-up supportive supervision was provided on-site.
Reinforcing activities to strengthen malaria laboratory diagnosis in these facilities will continue, and expansion to additional health facilities in malarious area of the country needs to be pursued. Improving the quality of malaria laboratory diagnosis plays a pivotal role in minimizing misdiagnosis, over-diagnosis, inadequate and inappropriate treatment and drug resistance, thus improving the overall effectiveness of malaria prevention and control efforts.
This piece was originally posted on the President's Malaria Initiative website.







Comment
Make a general inquiry or suggest an improvement.