 Dr. Margaret Chan
WHO
Dr. Margaret Chan
WHO
 Dr. Margaret Chan
WHO
Dr. Margaret Chan
WHO
FrontLines: How does WHO work with USAID to deliver health services to developing countries?
Chan: WHO has long worked closely with USAID in a number of areas. Let me give just a few of many examples.
USAID has supported WHO in seeking practical solutions to the current severe shortage of health-care staff. This work, in turn, has improved coverage with antiretroviral therapy for HIV/AIDS in several African countries.
USAID has given WHO tremendous support in TB (tuberculosis) control, especially for laboratory work and including support for the introduction, together with field-level evaluations, of an impressive new diagnostic test that takes 100 minutes to produce results compared with the usual two-to-three months. This new tool promises to revolutionize TB care in resource-poor settings.
Equally important is USAID’s financial support for work in strengthening health systems in some of the world’s most needy, and most challenging countries, building on WHO’s on-going work in this area. Apart from rehabilitating health facilities and laboratories, this support has strengthened capacities to respond to outbreaks of infectious disease, thus contributing to wider health security for neighboring countries.
FL: Roughly 80 percent of people in the developing world do not have access to health facilities. What is the most effective way we can help these individuals access quality care, even in rural and low resource settings?
Chan: In my view, the best way is to go back to the basics: the values, principles, and approaches of primary health care. Abundant evidence, over decades of experience, supports this view. Countries at similar levels of socioeconomic development achieve better health outcomes for the money when services are organized according to the principles of primary health care. A revitalization of primary health care is the smart move to make.
To be frank, a smart move, in this case, is not an easy move. We are almost starting over from scratch. Over the past three decades, health systems in large parts of the developing world have crumbled from neglect. Countries and their development partners have failed to invest adequately in basic health infrastructures, capacities, and services, including staff education and training, regulatory capacity, procurement systems, and statistical services.
Let me give just two examples. One, in 2006, WHO documented a stunning worldwide shortage of nearly 4.3 million doctors, nurses, midwives, and other health-care personnel, with the shortage greatest in sub-Saharan Africa. And, two, today, some 85 countries, representing 65 percent of the world’s population, do not have reliable cause-of-death statistics. This means that causes of death are neither known nor recorded, and health programs are left to base their strategies on crude and imprecise estimates.
For these and other reasons, many health systems are just barely able to cope with episodes of infectious illness. They are totally unprepared to cope with the onslaught of demands on staff, budgets, medicines, supplies, and hospital beds that comes with the rise of chronic non-communicable diseases. In an alarming trend, developing countries now bear nearly 80 percent of the burden of deaths from diseases like cardiovascular disease, diabetes, and cancer. In poor and disadvantaged groups, patients with these diseases fall sicker sooner and die earlier than their counterparts in wealthier societies. Primary health care has been identified as by far the best framework for preventing and managing these chronic conditions at both the population-wide and the individual level.
FL: In 2009 you gave a speech titled, Why the World Needs Global Health Initiatives in Venice, Italy. You stated that single-disease initiatives and health system strengthening are not mutually exclusive; rather they are mutually reinforcing. Can you talk about why integration is so important to strengthening health systems?
Chan: We do need both. The first decade of this century saw the establishment of numerous global health initiatives, including the Global Fund, the GAVI Alliance, PEPFAR (President’s Emergency Plan for AIDS Relief), and the U.S. President’s Malaria Initiative, and several innovative financing instruments. Most were created to support achievement of the health-related Millennium Development Goals. Nearly all focused on the delivery of commodities like medicines, vaccines, and bednets for individual diseases. All depended on a well-functioning health-care system to achieve their objectives, yet few initially made the strengthening of health systems an explicit objective.
Progress towards the health-related MDGs stalled, despite these initiatives, powerful interventions, and the cash to buy them in unprecedented quantities. Weak health systems were identified as the biggest obstacle to progress, especially in reducing maternal and childhood mortality. The need to strengthen health-care systems is now broadly acknowledged, also in the U.S. Global Health Initiative, and primary health care is regarded by many as the best framework for doing so.
The reduction of poverty is the over-arching objective of the MDGs. Progress is not measured by national or global averages, but by how well the health of the poor improves. If we miss the poor, we miss the point. A health system that lacks commodities for managing high-mortality infectious diseases and the main killers of mothers and young children will not have an adequate impact. By the same token, even the best-stocked delivery system will have an inadequate impact if it fails to reach the poor. As I said, we need both.
The momentum and drive of the global health initiatives have made specific weaknesses in health systems much more visible. This, in turn, has allowed a more precise definition of problems and a more targeted approach to solutions. In addition, these initiatives have reduced drug prices, rationalized the switch to second-line treatments, and exploited advances in information and communications technologies. They have upgraded the quality of clinical care with quality-assured interventions and standardized treatment protocols, setting a new benchmark for global health.
FL: If done correctly, why is development assistance not charity? Along the same lines, why is country ownership so important?
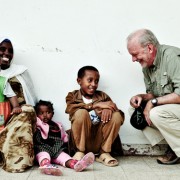
Chan: Countries want capacity, not charity. They want a hand up, not a hand-out. Good development assistance is a mutual undertaking, not the generous and warm-hearted giving by the wealthy to the poor and needy. It accepts the recipient country as an equal partner. Good aid for health development aims to build self-reliance. It does so by channeling support in ways that strengthen existing infrastructures and capacities, whether for data collection and monitoring, drug procurement and distribution, or financial management of projects. If aid does not explicitly aim for self-reliance, the need for aid will never end.
Dependency negates dignity. Hand-outs steal hope. Hopelessness stifles that fundamental human aspiration for a better life, and the willingness to work hard to get there. Children inherit their parents’ poverty, misery, and ill health. Ill health saps productivity. The costs of care trap the next generation in poverty. It never ends.
Country ownership of the health agenda is the surest route to self-reliance and sustainable results. Country ownership increases the legitimacy of government in the eyes of its citizens, and encourages accountability.
The launch last December of a new vaccine to prevent epidemics in Africa’s meningitis belt provides a good example. The vaccine was developed in response to the expressed needs of African leaders, including an affordable price. The project was coordinated by WHO and PATH, with core funding from the Bill & Melinda Gates Foundation and additional support from USAID and others. A consortium of academics and scientists developed the vaccine, with technology transferred from the U.S. and the Netherlands to the Serum Institute of India, which agreed to manufacture the vaccine at the target price of 50 cents per dose. African scientists contributed to the design of study protocols and conducted the clinical trials. At every stage, this was a process of shared goals and mutual learning. African countries frequently have to wait years, if not decades, for new medical products to trickle into their health systems. For once, the best technology that the world, working together, can offer was introduced in Africa.
FL: Is there one example that stands out to you that demonstrates the immense need for continued innovation in health for development?
Chan: New vaccines nearly always give public health its biggest leap forward. Of course, everyone would love to see a vaccine developed for the high-mortality killers, like HIV and malaria, and a better vaccine for tuberculosis. Work in this direction is already under way, largely through public-private partnerships and often with generous funding from the Bill & Melinda Gates Foundation.
But on a more immediate level, what we need most is to see existing technical interventions adapted to meet the reality of conditions, and resources, in the developing world. For example, products that can be administered safely by non-specialist staff help compensate for the shortage of skilled health-care workers. Products made suitable for home-based care are important for diseases like malaria, which can kill within 24 hours of symptom onset.
Simplified packaging or treatment regimens increase patient compliance, especially when health literacy is low. Simplified point-of-care diagnostic tests can help bring care closer to homes. Better diagnostic tools also contribute to the more rational use of drugs, and can help delay the development of drug resistance.
Robust products that resist heat and humidity offer advantages in tropical areas poorly served by electricity supplies. These are the so-called “hot medicines” that break the cold chain requirements. For example, lives could be saved by the development of heat-stable insulin for diabetes and a heat-stable oxytocin for the management of postpartum hemorrhage.
This is one complaint I hear repeatedly from health officials in developing countries. Their health problems are neglected by R&D (research and development), and when new tools become available, they are nearly always priced beyond reach.
FL: Improving health, in a general sense, is far from simple. But what are some of the simplest ways to see real health gains in the developing world?
Chan: This question deserves a simple answer: educating girls and empowering women. Nothing pays a bigger dividend, and it keeps paying back, from one generation to the next.
Another simple tool, with a lot of complex work behind it, is the WHO Model List of Essential Medicines, which helps countries invest precious resources on medicines that match priority health needs and bring the biggest population-wide gains in health outcomes. In times of financial austerity, tools that help rationalize health expenditures become all the more important.
Approaches that genuinely engage communities can produce indigenous, ingenious solutions that work better than high-cost technology. This is true for Community Led Total Sanitation, an innovative methodology for mobilizing communities to completely eliminate open defecation. The approach offers no subsidies, no pre-cooked solutions, no high-tech marvels, but it has already begun to revolutionize rural sanitation in large parts of Asia and Africa.
FL: You’ve argued that the public health landscape is crowded, and governments, philanthropists, NGOs, and the private sector scramble, sometimes haphazardly, to attain health goals. Is there a main way that in your opinion would make development assistance more effective?
Chan: The International Health Partnership Plus is addressing the need to harmonize development assistance and reduce the current waste, duplication, and high transaction costs.
The Paris Declaration on Aid Effectiveness, and the related Accra Agenda for Action, are useful policy instruments that set out the mutual responsibilities of donors and recipient countries. They represent a new kind of thinking: donor policies and practices can themselves make aid ineffective, diminishing the power of investments to bring real and measurable improvements in health outcomes. These instruments encourage donors to align their work with the health priorities and capacities of recipient countries. In other words, to put countries in the driver’s seat.
This is where all of us need to do more work. WHO has a country office in nearly every developing country, usually located close to the Ministry of Health. Staff in these offices need to do much more to help ministries of health strengthen their national health plans and strategies and then negotiate with development partners to support these priorities and follow these plans.
Waste and duplication are also reduced when a health problem has a very strong technical strategy, with a good track record that is widely appreciated and embraced by development partners. The Stop TB Strategy, which has been strongly supported by USAID, provides a good example. The strategy has a plan, with budgeted activities, a strong partnership, and detailed technical guidance from WHO.
MeChanisms are in place to facilitate the procurement of quality-assured drugs at the best possible prices, including drugs for resistant forms of TB. Implementation, monitoring, and reporting take place in the context of the country-led framework of national TB programs. In this case, a strong and explicit technical strategy helps ensure that various NGOs, aid agencies, and other partners will play their strengths to the same script. That stops the scrambling.
FL: Where, in your opinion, have the greatest gains towards achieving the Millennium Development Goals been made?
Chan: Since the start of this century, the number of under-5 childhood deaths dropped below the 10 million mark for the first time in nearly six decades, dropped again to below 9 million, and now stands at just above 8 million.
The number of people in low- and middle-income countries receiving antiretroviral therapy for AIDS moved from under 200,000 in late 2002 to more than 6 million today, an achievement unthinkable a decade ago.
The rate of people newly ill with tuberculosis peaked and then began a slow but steady decline. For the first time in decades, we are seeing signs that the steadily deteriorating malaria situation might be turned around.
Progress in controlling the neglected tropical diseases has also been impressive. By the end of 2008, some 670 million people had been reached with preventive chemotherapy for at least one of these diseases. Cases of guinea worm disease are at their lowest level ever, now confined to only four countries.
I think the message is clear: Increased investment in health development works. But it has to keep on working, even in an era of financial austerity. With the sole and rare exception of disease eradication, the work of public health is never done.
FL: Even people outside the global health community know about HIV/AIDS, malaria, pneumonia, polio. What would you say is the greatest issue or obstacle to global health that doesn’t necessarily make headlines?
Chan: The fact that health systems throughout much of the developing world have crumbled to the point that they are barely able to function. In my view, this is the biggest obstacle to better health.
This has zero news appeal for the media and little attraction for donors. Donors want quick and measurable results. Building a health system takes time, and improvements are difficult to measure. But this is the one area where investments are most desperately needed. As we have learned, even the most powerful interventions will see their impact blunted in the absence of a well-functioning health system.
Health systems are social institutions. They do far more for society than deliver babies and pills, like a post office delivering parcels. Properly managed and adequately financed, a fair and equitable health system contributes to social cohesion and stability. A world that is greatly out of balance in matters of health is neither stable nor secure.
Let me give just two examples of the challenge. The difference in life expectancy between wealthy and poor countries now exceeds 40 years. Yearly government expenditures on health range from as little as $1 per person to nearly $7,000. Given the extreme nature of these imbalances, visible with the click of a computer mouse, should anyone be surprised when social unrest seethes?










Comment
Make a general inquiry or suggest an improvement.