Team members from Sisu Global Health first witnessed the “soup ladle” method at a hospital in Ghana - a very unsterile and unsafe method for blood autotransfusion. Autotransfusion, a standard practice in the United States, recycles a person’s own blood in cases of significant blood loss. Autotransfusion can also aid in cases of large internal bleeds where donor blood is scarce. Autotransfusion technology is too costly for many low-income countries and lack of access to blood is a major contributor to unnecessary maternal deaths in the developing world.
“Right now, across parts of Sub-Saharan Africa, people are literally using a kitchen soup ladle and cheese cloth to salvage blood,” says Carolyn Yarina of Sisu Global Health.1 The team was struck by this “soup ladle” method as they watched the process in Ghana and saw how the doctor opened the woman’s abdomen, scooped out blood using a ladle, filtered it through gauze and poured into a pre-cut blood bag to reinfuse to the patient. This unsanitary method greatly increases risk of blood contamination and clinician health.
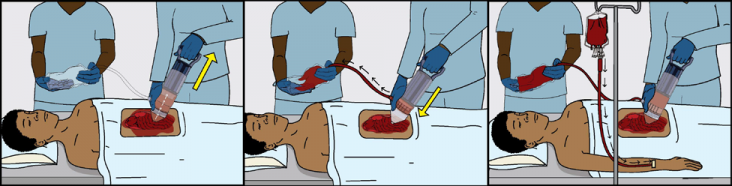
Sisu Global Health, the women-led small business located in Baltimore, Maryland, wanted to come up with an accessible and safer solution to use in place of donor blood and the “soup ladle” method. They decided to design an innovation to treat ruptured ectopic pregnancies, occurring when the fertilized egg is situated outside of the uterus. As the egg grows, there is a high chance that it will burst through the local vessels and cause a massive, life-threatening bleed. They designed a simple device, known as Hemafuse, to salvage and recycle a woman’s own blood during internal bleeding. The device is an affordable, handheld tool that is designed to be a faster and safer alternative to the “soup ladle” method. The device functions like a syringe and when the handle is pulled up, blood is pulled through a filter. The special design of the filter removes blood clots and other impurities. When the handle is pushed down, the blood is then pushed through tubing into a blood bag. The blood bag is then connected to the patient to be re-transfused.2
The Sisu team applied to Saving Lives at Birth in 20 14 and won a grant for a feasibility study in Ethiopia. The study showed that the Hemafuse is a safe device for collecting and reusing blood. Katie notes that Saving Lives at Birth and its partners have been crucial in validating the work they are doing and offering a supportive network to the company. “Receiving the Saving Lives at Birth award was the first time that the Hemafuse was seen as something valuable to the outside world,” Katie says. The company also received support from groups like VentureWell, a private company that works with innovators to help bring ideas to market, and leveraged $1.2 million dollars of additional funding to help further develop the Hemafuse. Thanks to Saving Lives at Birth, Sisu has reconnected with VentureWell. Sisu has applied for another Saving Lives at Birth grant and is expanding use of the Hemafuse into Ghana and Kenya.
Kofi Effah, an autotransfusion specialist from Battor Catholic Hospital in Ghana says, “I think it is a great device. We have been looking forward to having something like this for many years and we see a lot of women with ruptured ectopic pregnancies who need blood. It is safer to have their own blood and sometimes we also have challenges with our blood bank, so if we could autotransfuse, this offers a safer approach than what we had been doing in the past.”3 Over the next 4 years, Sisu expects to impact 14 million lives with Hemafuse - including direct lives saved with the device as well as calculated donor blood saved that would contribute to other life-saving procedures.
« Back to the Acting on the Call home page
1 http://www.sisuglobalhealth.com/
2 http://www.sisuglobalhealth.com/hemafuse/
3 http://www.sisuglobalhealth.com/







Comment
Make a general inquiry or suggest an improvement.